Microsurgical Sperm Retrieval from the Testicle (Micro-TESE)
Azoospermia,is defined as the absence of spermatozoa in the ejaculate after assessment of semen on at least two occasions, is observed in approximately 1% of the population and in up to 15% of infertile men. Non-obstructive azoospermia (NOA), which is diagnosed in about 60% of azoospermic men, can be detected clinically in men with small-volume testicles, elevated follicle-stimulating hormone (FSH) and azoospermia.

Micro-TESE stands for Microsurgical Sperm Retrieval from the Testicle. This involves a small midline incision in the scrotum, through which one or both testicles can be seen.
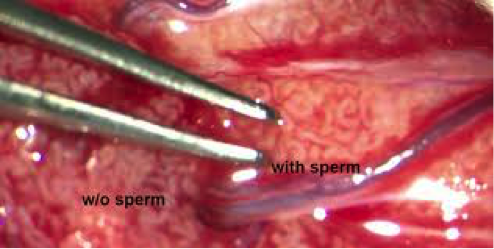
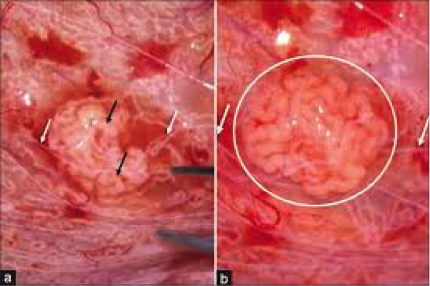
The surgeon examines the testicle(s) under the microscope, which provides up to 20x magnification, in search of areas where the seminiferous tubules – small areas of testicular tissue – are dilated and therefore more likely to contain sperm. The surgeon then removes these areas, and examined in laboratory for the presence of sperms.It allows the removal of tiny volumes of testicular tissue in areas of active sperm production by microscope, improving sperm yield compared to traditional biopsy techniques.
This approach has a number of advantages over other sperm retrieval techniques. It maximizes the yield of spermatozoa and minimizes the amount of testicular tissue required and vascular injury created, by making identification blood vessels easier.
Minimally invasive, safe and limits the disruption of testicular function. With micro-TESE, successful sperm retrieval has been reported in up to 63% of men, whereas conventional sperm retrieval procedures have reported success rates from 20% (percutaneous testicular biopsies) to 45% (open testis biopsies).
Sperm processing
The mechanical processing of testicular tissue samples in the operating room involves cutting tissue samples and passing the sample through a fine catheter. This process increases the yield of testicular by 300-fold, facilitating early identification of sperm in the operating room. Each specimen should be examined for the presence of sperm in the operating room; the procedure is terminated once sperm are found. Sperm are not always identified in the operating room; meticulous laboratory-based, including enzymatic treatment is performed to improve the chances of finding sperm. The chance of finding spermafter chemical digestion when sperm were not initially found is 25%–30%.
Although men with NOA have different pathological patterns that can be treated with this approach, the technique of finding areas of the testicle with sperm production is important in determining the success of an IVF cycle. Multiple techniques for sperm retrieval have been described including fine needle aspiration (FNA), percutaneous testis biopsy, open testicular biopsy or testicular sperm extraction (TESE) and microdissection testicular sperm extraction (micro-TESE).
While the success of micro-TESE compared to other sperm retrieval techniques has been accepted, prediction preoperativelyto whom the procedure willto be successful remainscontroversial. Preoperative variables such as age, FSH, testicular volume, inhibin B, genetics, Klinefelter syndrome, history of varicocele,cryptorchidism, as well as intaoperative variables such as histopathology and tubular diameter . These variables were determined by reviewing the available literature on prediction of success in sperm retrieval techniques, with a focus on those reviews that are dedicated to micro-TESE.
Previous biopsy
A single biopsy is inadequate to retrieve sperm and more extensive testicular evaluation may be needed before sperms are found. Multiple random biopsies will carry the risk of creating intratesticular scar, decreasing androgen levels and future sperm production. A diagnostic testicular biopsy provides limited evaluation of testicular function; it cannot determine which men with NOA will have successful sperm retrieval. Patients who undergo one to two biopsies with no spermatozoa identified, the success rate of micro-TESE is close to 60%. There is no threshold for the number of negative biopsies that permits sperm retrieval using micro-TESE.For men who had previously conventional TESE and fail to have sperm retrieval, a repeat conventional TESE causes further testicular damage with limited success. In case of a failed conventional TESE, micro-TESE can be offered and spermatozoa retrieval is possible with sperm retrieval rate of 45%. Previous micro-TESE seems to have little effect on the success of future microdissection. A repeat micro-TESE in men who underwent one successful microdissection attempt carries a sperm retrieval rate of 82%. If a complete micro-TESE procedure is done by examining the deeper tissues of the upper and lower poles of both testes, the operation should not be repeated. Sperm retrieval rate for repeating previously failed ‘micro-TESE' procedures done elsewhere is 10%.
A high sperm retrieval rate with micro-ESE is clearly demonstrated in men with Klinefelter syndrome, cryptorchidism, and prior history of chemotherapy and Y chromosome microdeletions as well as idiopathic NOA. It is possible that the chance of sperm retrieval rate can be maximized by pre-treatment of patients to optimize hormonal levels, especially in men with Klinefelter syndrome.
Follicle-stimulating hormone (FSH)
Follicle-stimulating hormone (FSH) is a glycoprotein produced in the pituitary gland .Many theories suggest that FSH may be useful in predicting the outcome of sperm retrieval procedures, in that patients with very high levels of FSH would tend to have a global failure of sperm production within the testis.
While the success of micro-TESE compared to other sperm retrieval techniques has been accepted, a full understanding of predicting preoperatively to whom the procedure will to be successful remainscontroversial. Preoperative variables such as age, FSH, testicular volume, inhibin B, genetics, Klinefelter syndrome, history of varicocele, cryptorchidism, as well as intaoperative variables such as histopathology and tubular diameter . These variables were determined by reviewing the available literature on prediction of success in sperm retrieval techniques, with a focus on those reviews that are dedicated to micro-TESE.
Post-Surgery
Most men are surprised by the minimal pain they have after this surgery. The scrotum is one of the fastest healing parts of the body and theclosure of the layers used helps to ensure that men do not have infections or bleeding after the surgery.
Most men use an ice pack for the first 24 hours after the surgery with no need of analgesia later. Men are advised to avoid sex, masturbation, or vigorous exercise for 10 days after the surgery. It typically takes 10–14 hours of searching for sperm under the microscope to determine if any sperm were found.
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
