Epidural Analgesia In Labour Indications, Various techniques its advantages and Contraindications
when to have lumbar epidural analgesia
- Pain
- Pre-eclamptic toxaemia
- High risk fetus group
- Breech delivery/ twin delivery
- Trial of prolonged labour
- Patient request
- Symptomatic heart disease
- Respiratory disease
- Cerebrovascular disease
- Abnormal or dead fetus
- Inco-ordinate uterine action
Prerequisites for epidural
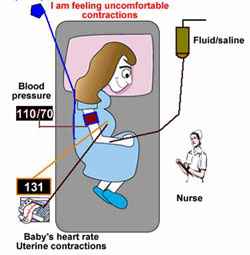
- Maternal consent
- Maternal /fetal status
- Progress of labor
- Nursing
- IV bolus
- Monitor B/P
- Continuous fetal monitoring
- Catheter
- Safety
- Muscle weakness
Epidural Analgesia
-The Most effective form of pain relief for labor.
- Opioids Combination with low concentrations of local anesthetics provided effective analgesia whilst reducing some of the unwanted side effects such as a motor block
Extradural analgesia advantages over subarachnoid block
- Amount of and Incidence of maternal arterial hypotension is less
- Incidence of post puncture headache and serious neurological sequel are less
- It is safer in theory to use the continuous technique in the extradural space than in the subarchnoid space.
Different techniques of Extradural analgesia
- Lumbar epidural block
1. Standard block T10 to S5
---A - Single Dose
---B - Continuous Technique: Repeated Injection Through Catheter
2. Continuous segmental block,
---A - Initially Segmental T10 To L1 Block
---B - In Second Stage Extended To Sacral Segments
- Caudal block
- Single dose
- Continuous technique
- Double catheter technique
- Upper catheter for segmental block
- Lower catheter for sacral block
Advantages of Epidural Analgesia
- It gives superior pain relief during first and second stages of labor.
- mother cooperation during labor and delivery will be easier.
- It gives anesthesia for episiotomy or forceps delivery
- extending of anesthesia for cesarean delivery is possible.
- opioid -induced maternal and neonatal respiratory depression will be avoided.
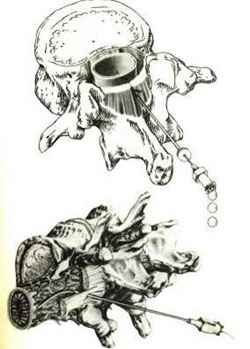
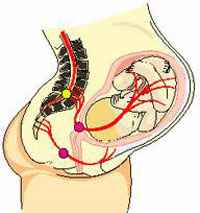
How does the epidural anesthesia work ?
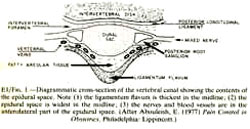
- An epidural anesthetic blocks the nerve roots that lead to the uterus and lower half of the body. The roots are located in a space near the spinal cord (epidural space). Which lies within the spine just outside the outer covering of the spinal cord.
Epidural Block
- Continuous block
- Lies between Dura mater and ligamentum flavum
- Does not enter CSF space
- Give the bolus- observe for hypotension
- Change position frequently
- respiratory depression can result if narcotics are used
Contraindication to epidural analgesia
- Patient refusal
- Active maternal hemorrhage
- septicemia in the mother or untreated febrile illness
- Infection at or near needle insertion site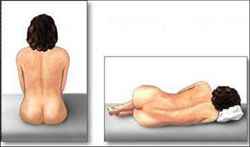
- If there is maternal coagulopathy (inherited or acquired)
Anatomy of epidural space
THE PROPER POSITION OF THE PATIENT TO APPLY EPIDURAL CATHETER
Epidural Procedure done by Dr. Najeeb Layyous in 1982












ANATOMICAL CONSIDERATION
- PAIN IN EARLY 1st STAGE :- T10 – Ll
- PAIN IN LATE 1st STAGE AND IN 2nd STAGE :- T10 - Ll AND S2 - S4
Physiology of labor pain(1st. stage
- Lower uterine segment distention,
- Mechanical dilatation of the cervix
- And due to stretching of excitatory nociceptive afferents resulting from the contraction of the uterine muscles.
Timing Consideration for epidural block
- Cervical dilation 3-5cm.
- Diagnosis of active labor has been established, and the patient has begun to request pain relief.
Epidural anesthetic agents

- The mostly used drugs are lidocaine 1 – 2 % for short or intermediate action.
- Bupivacaine 0.25 - 0.75 % for long action . Ropivacine 0.2 – 1.0 % for long action.
Epidural anesthetic agents
- The adult dose 1 -2 ml / segment bolus for anesthesia, the dose decreases with pregnancy and age, increases with height. - third or half of the initial dose can be re- injected when needed. - Test dose (3-5 ml) must be injected first to be sure of the proper space. - Opioids (morphine 2 -5 mg, fentanyl 0.05 – 0.1mg( may be added to local anesthetic drugs for epidural anesthesia.
Complications of epidural analgesia
Immediate
- Hypotension (systolic blood pressure <100 mm Hg or a decrease of 25 percent below pre-block average)
- Urinary retention
- Convulsions*induced by local anesthetic
- Cardiac arrest*induced by local anesthetic
Delayed
- Postural puncture headache
- Transient backache
- Epidural abscess or meningitis*
- Permanent neurological deficit* is very rare
- Epidural abscesses; extremely rare
Fetal Complications of epidural
- Hypotension ;
- May cause fetal distress and if not corrected within 3 minutes may lead to neurological sequalae and low APGAR
- Fever
- May result in unnecessary septic work up investigations for the newborn
Lumbar epidural analgesia Complications
- Headache - backache
- Haemorrhage
- Respiratory depression
- Retention of urine
- Infection
- Fetal depression from local anaesthetics - total spinal block
- Convulsions*induced by local anesthetic
- Cardiac arrest*induced by local anesthetic
- Epidural abscess or meningitis*
- Permanent neurological deficit* is very rare
Combined spinal epidural anesthesia.
- Also known as needle through a needle technique
- Introduced in the 80’s
- Epidural needle inserted, followed by a spinal needle is introduced through it into the subarachnoid space and an opioid or local anesthetic is injected, needle then withdrawn and epidural catheter inserted for top up doses when needed.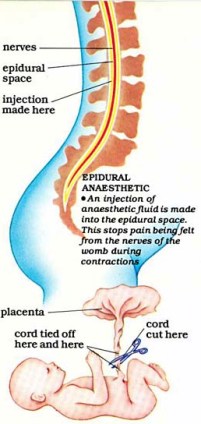
- Opioids given intrathecally or epidurally to cover the first stage of labor
- For the second stage of labor a local anesthetic is required
- A mixture of sufentanil with bupivacaine is given to cover early and late stages of labor with mild motor block, faster labor and less instrumental delivery rate
Why combined procedure is better than epidural?
- More rapid onset
- The anesthetic blood level is less in maternal and fetal serum
- More intense motor block for c/s
- Asserting the position of the epidural catheter
- Allows extension of sensory level or duration of spinal block; for a trial of forceps to c/s.
- The use of different agents later on in the post- operative period; pain relief is possible.
Combined spinal epidural
- Confirming the site of epidural catheter decreases the risks of dural puncture
- Not suitable for patient; if labor progresses rapidly this leaves the epidural catheter untested should an emergency rise requiring its immediate use for a c/s.
Spinal anesthesia complications
- Hypotension; due to sympathetic block. Which Is Treated By Uterine Displacement, Hydration And Ephedrine (10-15 Mg) I.V.?
- Total spinal block; due to overdose. Symptoms include hypotension, apnea and cardiac arrest!!!
- Spinal post puncture headache; it occurs in 1.5% of cases if the gauge 22-24 needle used. A result from CSF leak and prevented by using small gauge needles; placing the woman flat on her back for several hours post- procedure and avoiding multiple punctures.
- Convulsions; resulting from CSF hypotension
- Bladder dysfunction
- Hypertension with oxytocics used postpartum is seen more commonly in females who received regional anesthesia
- Arachnoiditis & meningitis; it used to occur due to preservatives found in anesthetics; nowadays, a rarity.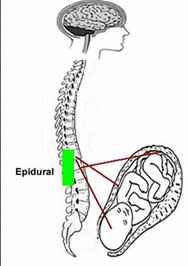
How epidural Affect labor and delivery
- No effect on the conduct of labor
- Increase the rate of instrumental delivery.
- Prolongation of second stage; allow the fetal head to proceed and crown spontaneously without necessitating bearing down provided fetal heart monitoring is reassuring.
- Rate of malposition and malpresentation are increased with epidural due to the decreased tone of the pelvic floor muscles and subsequently malrotation of fetal head and increased incidence of deep transverse arrest
- Early bearing down result in obstructed labor and requires intervention.
- When full dilatation allowed fetal head to descend, rotate and flex without undue bearing down.
- Remember mothers can’t feel the pushing to so allow the head to push down against the pelvic floor to be delivered
- Keep in mind!!!!! Crowning needs time; allow 3 hrs in primigravidas and 2hrs in multgravidas as long as the fetal heart is “ok”
How to avoid instrumental delivery
- Try not to give top up doses after full dilatation (at the expense of feeling pain in second stage)
- Limit the dose given of the local anesthetic close to the end of the first stage
- Avoid the urge to crowning the patient, as soon as she reaches full dilatation. Allow spontaneous descent of the head
- There’s no difference (as shown in studies) in the apgar scores amongst those who are allowed delivery without urging to push down early and those who deliver via instrumental delivery early after full dilatation
- Active management of the second stage of labor;
- make sure that there are good effective uterine contractions
- Encourage mother to push with uterine contractions
- Selective epidural block of the lower thoracic segments only which also covers perineal sensation whilst preserving pelvic floor muscle tone
- Caudal and lumbar epidural effect leads to absent or diminished bearing down reflex thus increased rate of instrumental delivery
- Give a segmental epidural at the level of t10-t12 that pertains to the bearing down reflex
- If you give analgesics with the anesthetic, you will decrease the dose of the anesthetic used thus the motor block,and its side effects are decreased
Baby Names Book, Arabic Baby Names
http://www.babynamesbook.net/
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
