Menopause, causes, clinical features, and management modes of treatment
The term means the ending of menstrual cycles, which is the central external marker of human fertility and occurs after six months of secondary amenorrhea in women aged 45 years or older.
It is a transitional phase from fertility to infertility state.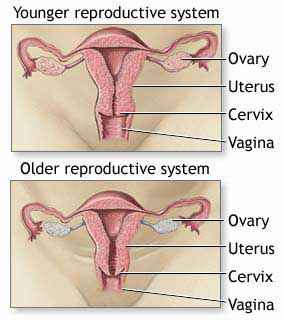
What leads to menopause is the depletion of oocytes and primordial follicles from the ovaries and the subsequent cessation of estrogen production.
The cessation of cyclic bleeding may take many forms;
The menstrual cycle may cease abruptly or may stop after a stage of polymenorrhea followed by a stage of oligo menorrhea.
Other causes of menopause :-
1- Surgical menopause :-
Surgical removal of both ovaries for any reason, like ovarian cancer.
Studies have indicated the median age of menopause in hysterectomized patients can be given at time of operation; indicating which patients may or may not be affected.
2- Premature ovarian failure (POF):-
Secondary amenorrhea due to ovarian failure may occur at any age, and if below age, 45 years may be accounted as premature, these patients exhibit low plasma estrogen, increased level of follicle stimulating hormone (FSH) and (LH). (POF) is associated with other autoimmune endocrinopathies and in about half of the patients other antibodies are present.
3- Radiation and chemotherapy:
Treatment of malignant disease in young women may provoke menopause in two ways; in women with breast cancer treated with radiotherapy, menopause may still be used to suppress estrogen output, and the use of chemotherapeutic agents in breast cancer or lymphomas may suppress and indeed arrest ovarian cyclic activity.
Symptoms of menopause
 1- Vasomotor symptoms:
1- Vasomotor symptoms:
The most noticeable consequences of the drop in estrogen levels are vasomotor symptoms in the form of hot flushes and night sweats. These are common and occur in at least 70-80% of women.
Their frequency may vary between a few to several dozen attacks per day, and the duration may be from a few weeks to many years.
2- Insomnia
Patient may experience repeated awakening from sleep with consequent loss of sleeping-hour quantity and quality.
3- Psychological symptoms, including:
Mood swings, anxiety, lack of concentration, depression, and loss of short-term memory.
4- Vaginal dryness :
Estrogen deficiency results in epithelial and connective tissue atrophy in the vaginal wall, causing vaginal dryness and dyspareunia.
5- Urinary symptoms:-
Estrogen deficiency results in atrophy in the urethral wall, predisposing to stress incontinence and atrophy in the trigone area of the bladder, resulting in urgency and urge incontinence.
6- Osteoporosis :-
In the early post-menopausal years the density of bone in women decreases at a faster rate than at any other time with greater bone resorption to the formation ratio.
In many women, this process results in osteopenia which strongly predisposes to fractures.
By the age of 70, 25% of women will have vertebral fractures, 15% will develop hip fractures, and 15% will develop fractures of the wrist.
Risk factor for osteoporosis:
1- Family history of osteoporosis
2- Smoking, alcohol abuse
3- Early menopause
4- History of prolonged immobilization
5- Treatment with corticosteroids or heparin
6- Medical conditions; hyperthyroidism, Cushing's disease, chronic renal failure, and hepatic insufficiency
7- Black women are less likely to develop osteoporosis than white or Asian women.
Thin women are more prone to osteoporosis than fat women.
Cardio vascular system:
The function of the heart and great vessels is now known to be affected by the presence and absence of estradiol.
- The incidence of myocardial infarction is much lower in pre-menopausal women than in men of the same age. The decline in plasma estrogen results in changes in lipid profile with promotion of both atherogenesis and vasoconstriction as estrogen exerts direct effects on the vessel wall.
Dietary changes and menopause
Diet is thought to be one factor that helps in the explanation of the cultural differences in the menopausal symptoms.
Asian women experience fewer menopausal symptoms and lower rates of hip fractures than Western women. This is related to their diets, which contain high levels of phytoestrogens (naturally-occurring estrogens), about 200 mg daily as compared to Western diet.
Phytoestrogens are structurally similar to estradiol but much weaker than the body's natural estrogen and have a cumulative effect when taken in sufficient amounts.
Soybeans are the richest source of this substance. In the USA, studies found that foods and drugs containing specific amounts of soya protein can lower cholesterol and improve arterial function, reduce atherosclerosis, then reduce cardiovascular disease.
Studies have not shown any significant adverse effects due to phytoestrogens. They are well-tolerated and in spite of their cost, they are very popular supplements.
Some studies have suggested that multivitamins and mineral supplements can reduce hot flushes, but their effect may be partly dependent on the quality of the woman's diet.
Supplementation of vitamin E 440-1200 I.U. daily reduces vasomotor symptoms.
Women in menopause and not on HRT (hormone- replacement therapy) are recommended to include 1500 mg of calcium daily.
Some clinicians would recommend adding vitamin D 400 IU daily with calcium, which significantly reduces fracture risk.
Exercise in menopause :
Exercise is effective in slowing the gradual, long-term aging-related bone loss and is important to cardiac health, helping to reduce weight, blood pressure, and cholesterol levels.
Women who are exercising regularly are less prone to suffer severe hot flushes and depression and have less insomnia, together with providing a greater feeling of well-being.
The safest exercise to recommend to women is walking.
Women who walk for at least one hour per week experience about half the coronary heart disease risk than women who do not walk regularly.
Hormone replacement therapies (HRT)
Hormone replacement therapies have been available for more than 25 years, and its use is growing rapidly.
HRT can effectively reverse all the effects of the menopause but should be given under medical supervision.
- Continuous estrogen- progestogen preparations:-
This type of therapy is taken every day without interruption and prevents endometrial proliferation. Their use, therefore, does not cause withdrawal bleeding, and the majority of postmenopausal women prefer a bleeding-free hormone treatment.
- Cyclic estrogen- progestogen preparations:-
In this type of therapy estrogen is taken for 21 days and is combined with a progestogen for the last 10 days following, which there is a four- to seven day medication-free interval during which withdrawal bleeding occurs.
This type relieves the symptoms effectively and regulates the cycle.
- Tibolone (Livial):-
This type of therapy is a synthetic steroid which exhibits estrogenic, progestogenic and androgenic activity, given in a dose of two to five mg daily to women at least one year after menopause and results in the suppression of symptoms and the prevention of bone loss.
This preparation is well-tolerated, and the amenorrhea which is present in 80% of patients by six months of use is usually warmly welcomed.
- Subcutaneous hormonal implants:-
This mode of treatment is restricted in the UK to patients who have undergone hysterectomy with or without oophorectomy.
The procedure involves the insertion of a pellet of estradiol in the subcutaneous tissue, usually of the lower abdomen, under sterile conditions and local anesthetic.
This implant usually is reviewed at six monthly intervals.
They are very well-tolerated and successfully treat menopausal symptoms and protect against bone loss.
- Transdermal estrogen:-
This type of therapy is particularly used in older women. Patches are available in varying strengths of 28 mg, 50, 75, or 100 mg of estradiol per day.
Seven-day patches are now available.
Skin reactions are minimal and such treatment is well-tolerated.
- Local estrogen:-
In this type of therapy estrogen is used in the form of cream, pessary, or vaginal ovules.
It is suitable for those women with local symptoms and in whom systemic administration of estrogen is hazardous.
Patients on HRT need a careful breast examination, pelvic examination, and blood pressure should be checked regularly along with a bone mineral density scan to check for osteoporosis.
The patient must be reviewed every three months, then at six-month intervals thereafter, and then annually.
Contraindications to Hormone replacement therapies (HRT) use:
. Absolute Contraindications to HRT
1- Breast cancer
2- Pregnancy
3- Endometrial cancer
4- Acute active liver disease
5- Uncontrolled hypertension
6- Confirmed venous thromboembolism
. Relative Contraindications to HRT
1- Presence of uterine fibromyomata
2- Past history of benign breast disease
3- Unconfirmed venous thromboembolism
4- Chronic stable liver disease
5- Migraine
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
