Uterine Abnormalities - Müllerian Ducts Abnormalities
Female genital tract developed from three origins:
1. Ovaries from the germ cells that migrate from the yolk sac into the mesenchyme of the peritoneal cavity and developed into ova and supporting cells.
2. Lower third of a vagina developed from the ascending Sino vaginal bulb.
3. 3- Uterus, fallopian tubes & upper two-thirds of the vagina developed from the fusion of two Müllerian ducts & this is our subject for discussion.
Complete formation of the genital tract depends on the completion of 3 stages.
• Organogenesis
If one of the tubes fails to develop, it results in the unicornuate uterus and if both failed then this will cause uterine agenesis or hypoplasia.
• Fusion
Two kinds of fusion
1. Lateral fusion process by which the two Müllerian ducts fuse together to form the uterus, tubes & cervix. Failure of this process cause bicornuate or didelphys uterus.
2. Vertical fusion: formation of the vagina completed by the fusion of the lower part of Müllerian duct that forms the upper two thirds and the ascending Sinovaginal bulb that forms the lower one third, incomplete vertical fusion lead to imperforate hymen.
• Septal resorption
Normally, the median part of the fused Müllerian ducts forms septum that resorpe to form single uterine cavity, failure of this resorption lead to septate uterus complete or partial.
Frequency of Müllerian Ducts Abnormalities
It occurs in 0.1_0.5%in healthy fertile population.
Clinical presentation of Müllerian Ducts Abnormalities
It differs in each patient according to the type of abnormality but nearly the most common presentations are.
• Infertility
• Recurrent abortion
• Preterm labor
• Intra uterine growth retardation
• Primary amenorrhea in imperforated hymen & haematocolpus
Diagnosis of Müllerian Ducts Abnormalities
Clinical history and physical examination cannot give much about the diagnosis, so the best way is by using imaging techniques: 
1. Hysterosalpingography
It has false-positive results of 38% and false-negative results of 28%. It also cannot assess the outer fundal contour making it impossible to differentiate between the septate and bicornuate uterus.
Special criteria put in mind to confirm the diagnosis by H S G.
- a- Intercornual distance (distance between the distal ends of the horns):
- - Less than 2 cm means septate uterus.
- More than 4 cm means bicornuate uterus
- Between 2 and 4 cm means normal uterus.
• Intercornual angle (formed by the most medial aspects of the two uterine hemi cavities)- - Less than 60 means septate uterus
- More than 60 means bicornuate uterus
• T shaped uterus means DES exposure - - Less than 2 cm means septate uterus.
2. MRI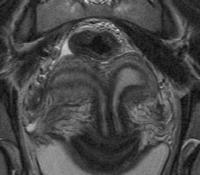
It allows imaging of the uterus in the coronal plane. It can assess the uterine cavity as well as the uterine contour, but it is coasty and requires referral to an imaging facility so the diagnosis will be delayed.
3. Three dimensional ultrasound
It provides information that is the same or better than that obtained with MRI and it’s less expensive than MRI, and readily available in most centers which enable expedited diagnosis.
When combined with saline infusion 3D ultrasound yield information similar to that obtained by HSG.
When scanning a gynecology patient, especially if a uterine abnormality is imaged, the kidneys need to be assessed.
 Uterine Septum with early pregnancy
Uterine Septum with early pregnancy Uterine Septum
Uterine SeptumClassification of Müllerian duct abnormalities. And its surgical treatment
Anatomy: Müllerian duct anomalies are categorized most commonly according to the American Fertility Society (AFS) Classification Scheme (1988 into 7) as follows:
1- Class I (hypoplasia/agenesis): This class includes entities such as uterine/cervical agenesis or hypoplasia. The most common form is the Mayer-Rokitansky-Kuster-Hauser syndrome, which is combined agenesis of the uterus, cervix, and upper portion of the vagina. Patients have no reproductive potential aside from medical intervention in the form of in vitro fertilization of harvested ova and implantation in a host uterus occurs in 15 to 40% and also sometimes skeletal abnormalities.
Diagnosis of vaginal agenesis
- presented as primary amenorrhea
- Normal secondary sex characteristics
- Pelvic examination reveals patulous urethra
- Vagina can be completely absent or shunt vaginal pouch can be present.
- Uterus cannot be palpated on rectal examination
- Ultrasound shows absent uterus and sometimes renal abnormalities
- Laparoscopy is not indicated unless the diagnosis cannot be determined by the above findings
- Treatment of vaginal agenesis
1. Non surgical treatment by using graduated dilators may take several months to few years before a functional vagina is formed so surgery remains the most effective method of treatment
2. Surgical treatment by vaginoplasty, the aim is to create a new vagina, surgical treatment should be considered only when the patient wishes to become sexually active and is highly motivated to use vaginal prosthesis for several months after surgery. there are various methods of vaginal reconstruction, some of these methods.
- Full thickness skin graft
- Transposition flaps.
2- Class II (unicornuate uterus): An unicornuate uterus is the result of complete, or almost complete, arrest of development of one Müllerian duct. If the arrest is incomplete, as in 90% of patients, a rudimentary horn with or without functioning endometrium is present. If the rudimentary horn is obstructed, it may come to surgical attention when presenting as an enlarging pelvic mass. If the contra lateral healthy horn is almost fully developed, a full-term pregnancy is believed to be possible (see didelphys uterus).
- Surgical treatment
Women with unicornuate uterus are not generally considered for reconstruction metroplasty. The only surgical indication is the presence of the endometrium in the accessory horn and this can be removed by laparoscopic hemi hysterectomy while the operation not indicated for rudimentary horn which lacks an endometrium.
3- Class III (didelphys uterus): This anomaly results from complete nonunion of both Müllerian ducts. The individual horns are fully developed and almost normal in size. Two cervices are inevitably present. A longitudinal or transverse vaginal septum may be noted as well. Didelphys uteri have the highest association with transverse vaginal septa but septa also may be observed in other anomalies. Metroplasty is Considered; however, since each horn, is almost a fully developed uterus, patients have been known to carry pregnancies to full-term; treatment is different according to the presentation.
a- Uterine didelphys with obstructed unilateral vagina: full excision on marsuplization of the vaginal septum. Also laparoscopy preferred to be done intra operatively to treat associated endometriosis or adhesions if present.
b- Uterus didelphys non obstructed: These patients are not candidates for surgical unification. Fortunately, they have had minimum associated problems and the fertility is good.
4- Class IV (bicornuate uterus): A bicornuate uterus results from partial nonunion of the Müllerian ducts. The central myometrium may extend to the level of the internal cervical os (bicornuate unicollis) or external cervical os (bicornuate bicollis). The latter is distinguished from didelphys uterus because it demonstrates some degree of fusion between the two horns, while in classic didelphys uterus, the two horns and cervices are separated completely. In addition, the horns of the bicornuate uteri are not fully developed; typically, they are smaller than those of didelphys uteri. Some patients are surgical candidates for metroplasty surgical treatment.
Although numbers of metroplasty procedures are available, the strassmann procedure is the surgical treatment of choice for unifying the bicornuate and didelphys uteri. This is simply explained by fusing the fundi of the uteri. If two cervices are present their unification is not recommended.
Hysteroscopy resection is contraindicated in this setting because it can result in uterine perforation.
5- Class V (septate uterus): A septate uterus results from failure of resorption of the septum between the two uterine horns. The septum can be partial or complete, in which case it extends to the internal cervical os histologically, and the septum may be composed of myometrium or fibrous tissue. The uterine fundus is typically conved but may be flat or slightly concave (<1-cm fundal cleft). Women with a septate uterus have the highest incidence of reproductive complications. Differentiation between a septate and a bicornuate uterus is important because septate uteri are treated using transvaginal hysteroscopic resection of the septum, while if surgery is possible and/or indicated for the bicornuate uterus, an abdominal approach is required to perform metroplasty.
Surgical treatment of Uterine Septum
The treatment of choice is transcervical lyses of the uterine septum combined with concurrent laparoscopy to reduce the risk of uterine perforation during septal incision.
The operation done by hysteroscopy, which is introduced through the cervix and the septum is cut and IUD is inserted and left for at least 2 months to prevent intrauterine adhesions formation. Others found this is unnecessary and may provoke local inflammation with subsequent synechiae.
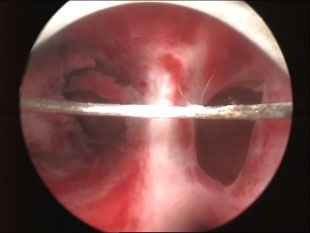
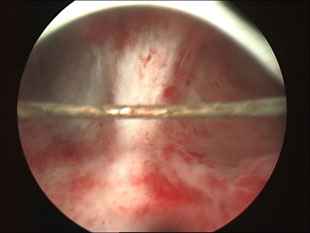
Intrauterine septum as seen by hysteroscopy
Hysteroscopic Septum Resection Video clips | Hysteroscopic Septum Photos
6- Class VI (arcuate uterus): An arcuate uterus has a single uterine cavity with a convex or flat uterine fundus, the endometrial cavity, which demonstrates a small fundal cleft or impression (>1.5 cm). The outer contour of the uterus is convex or flat. This form is often considered a normal variant since it is not significantly associated with the increased risks of pregnancy loss and the other complications found in other subtypes. This abnormality doesn't need any interference because researchers found that there is no difference in the reproductive outcome compared with normal.
7- Class VII (diethylstilbestrol-related anomaly): Several million women were treated with diethylstilbestrol (DES; an estrogen analog prescribed to prevent miscarriage) from 1945-1971. The drug was withdrawn once its teratogenic effects on the reproductive tracts of male and female fetuses were understood. The uterine anomaly is seen in the female offspring of as many as 15% of women exposed to DES during pregnancy. Female fetuses which are affected have a variety of abnormal findings that include uterine hypoplasia and a T-shaped uterine cavity. Patients also may have abnormal transverse ridges, hoods, stenoses of the cervix, and adenosis of the vagina with increased risk of vaginal clear cell carcinoma. Imaging findings are pathgnomonic for this anomaly).
Conclusion
Not all the types of uterine abnormalities can affect fertility and also not all the abnormalities correctable surgically. Uterine Abnormalities (Müllerian duct anomalies) are an uncommon but often treatable cause of infertility. Patients with Müllerian duct anomalies are known to have a higher incidence of infertility, repeated first trimester spontaneous abortions, fetal intrauterine growth retardation, fetal malposition, preterm labor, and retained placenta. The role of imaging is to help detect, diagnose, and distinguish surgically correctable forms of Müllerian duct anomalies from inoperable forms. In some correctable lesions, the surgical approach is altered based on imaging findings.
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
