Pelvic Adhesions And Infertility
Pelvic adhesions are fibrotic tissues or scars that develop in the pelvic cavity between the uterus, ovaries tubes, bowels and the bladder. Also, they can be found inside the tubes and the uterus. These adhesions can block or distort the tubes.
The formation and reformation of peritoneal adhesions is a common problem which causes a range of clinical symptoms in women including infertility.
Pelvic adhesions are responsible for 15% to 20 % of all infertility causes.
Tubal infertility accounts for 30% to 40% of the etiologic factors in female infertility
Incidence of Post-Operative Adhesions
It has been recognized that pelvic adhesions occur in 55% to 100% of women following a laparotomy. Until anesthesia and the development of antiseptic surgery had made laparotomy a practical, relatively safe and routine procedure, towards the last quarter of the 19th century, intra-abdominal adhesions appear to have been of little interest to clinicians.
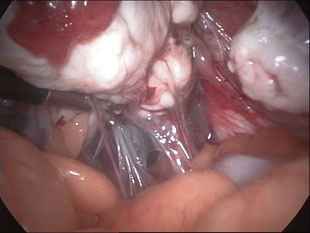
Increased awareness of peritoneal adhesions has encouraged the use of surgical techniques such as microsurgery and laparoscopy, designed to decrease peritoneal trauma.
Before laparoscopic surgery was introduced, microsurgical techniques had been developed, which introduced new concepts into operative surgery, giving respect for the delicate reproductive structures not found during old-fashioned laparotomy.
The main purpose of these procedures was to decrease the incidence of tubal and ovarian adhesions, by careful tissue handling, avoiding surface drying and giving meticulous attention to haemostasis.
Endoscopic surgery embraces the principles of microsurgery in that the large gas bubble formed by the pneumoperitoneum ensures adequate exposure and on holding the laparoscope close to the tissues, gives good magnification. In modern reproductive surgery, microsurgery means surgery of small structures that need magnification by glasses, microscope, or optic lenses such as those used during operative laparoscopy.
Pathophysiology of Adhesion Development
The peritoneum is composed of multiple layers. The first layer is the mesothelium which is the inner layer; the second layer is a layer of connective tissue, and a basement membrane. When the peritoneum is injured (which is inevitable during surgery), there is an inflammatory response where histamine and other inflammatory mediators are released from leukocytes and the mast cells. Dilatation of capillaries occurs and permeability increases. This lead to accumulation of white blood cells. Fibrinous exudate is thus formed at the site of injury. Lymphokines prostaglandins, bradykinin, serotonin, transforming growth factor and other chemotactic agents are present within the exudates material. Now, fibrinolysis will clear the exudates. So, plasminogen must be converted to plasmin by tissue plasminogen activator (t-PA). There is a constant balance in the system between tissue plasminogen activator and plasminogen activator inhibitors but, surgical trauma may have an inherent ability to decrease tissue plasminogen activity while increasing plasminogen activator inhibitors.

If the plasmin does not break the fibrin, the fibrinous exudate is converted into an organized adhesion and fibers of collagen are deposited. Then, blood vessels begin to form and lead to organization of the adhesion.
This process occurs over a one to seven day period of time. Usually the adhesions are complete within seven days. Then, Qualitative changes continue over the next months where the adhesions become more dense and vascularised.
Types of adhesions:
- Filmy adhesions: very thin and can be easily broken apart with gentle pressure
- Thick adhesions: often vascular and need energy to be removed like electrical or laser energy
- Band adhesions: string like bands between two or more structures
- Flat adhesions: result when two structures are stuck together
- Filmy adhesions: very thin and can be easily broken apart with gentle pressure
Tubal blockage versus adhesions:
It is important to distinguish between tubes that are blocked from those that are open but affected by adhesions. Blocked tubes occur when there is actual obstruction within the tube. A blocked tube can be diagnosed by hysterosalpingography. But adhesions can only be diagnosed with surgery to look inside the abdomen
Incriminated risk factors in the formation of pelvic adhesions
- Intra abdominal infection
- Tissue hypoxia or ischemia.
- May result from excessive tissue handling, suturing, crushing, ligating, cauterizing or peritoneum stripping
- Tissue drying.
- Presence of reactive foreign body. The common foreign bodies that may be introduced into the field during surgery include:
- sutures
- talc powder from surgical gloves,
- Lint from drapes, gowns, masks or laparotomy pads.
- Presence of intraperitoneal blood.
- Dissection of prior adhesions.
Causes of pelvic adhesions and tubal lesions
There are 3 main causes of pelvic adhesions and tubal lesions:
Pelvic infections
Surgical traumas
1. Pelvic infections (PID)
They are asymptomatic in 15% of cases. They are ascending or proximal (appendicitis). Chlamydia is responsible for 50% of cases. It causes adhesions and creates proximal or distal obstructions (phymosis, hydrosalpinx), and the lesions affect the mucous layers. Tuberculosis (genital) should not be forgotten.
2. Surgical traumas
The most traumatizing operations are: ovarian cystectomies, myomectomies, Ectopic pregnancy, Bowel surgery, and appendectomies. The last one appears to carry a risk of pelvic adhesions similar to that seen following gynaecological surgery.
Reconstructive Tubal Surgery: The repair of blocked fallopian tubes is a delicate procedure that often includes the removal of existing adhesions. Unfortunately, the surgery itself can also lead to the formation of new adhesions and infertility.
3. Endometriosis
The frequency of it being blamed for causing adhesions varies amongst authors (up to 40% in some series). Endometriotic nodules occur on the left tube, the ovary peritoneum and on the pelvic side wall.
Mechanisms resulting in Infertility
- The fallopian tube is a muscular organ that retrieves the egg from the ovary and transfers it toward the sperm. If the mobility of the tube is restricted by adhesions or if infection has stripped the cilia from the tubal lining, the tube cannot perform its function.
- Adhesions can block the passage of the ovum (egg) from the ovaries into the fallopian tubes.
- Adhesions around the fallopian tubes can interfere with sperm transport to the ovum through functional alterations, a reduction of the mobility of the tube.
- The disappearance of ciliation can also interfere with sperm transport to the ovum.
- Dysfunction of ovulation and immunitary phenomena as is the case in endometriosis
Falloposcopy (Tuboscopy)
Falloposcopy is a transvaginal micro endoscopic technique to explore the human Fallopian tube from the uterotubal ostium to the fimbrial end. Which may be used therapeutically for removal of debris and for cutting down filmy intraluminal adhesions?
Salpingoscopy
Salpingoscopy allows the ampullary mucosa to be visually inspected during either laparotomy or laparoscopy. The use of salpingoscopy may modify the management of patients with tubal infertility, since accurate evaluation of the endosalpinx allows us to identify the patients with a normal tubal mucosa:
76% to 80% of cases of periadnexal adhesions and 35% to 42% of cases of hydrosalpinx will benefit the most from tubal reconstructive surgery. In these patients, an intrauterine pregnancy rate equal to or higher than 70% may be expected following salpingo-ovariolysis and 60% following salpingostomy (Brosens, 1996; Marana et al., 1997).
Salpingoscopy should be carried out in all diagnostic laparoscopies and particularly in patients with tubal factors, to help in making the choice between surgical treatment and ART.
However, problems with availability of equipment (2.8 mm rigid salpingoscope that allows a detailed vision of the tubal ampullary mucosa) limits the use of this method in routine clinical practice.
Selection of candidates for surgery
Once diagnostic procedures have been performed and a therapeutic approach has been defined, patients must be fully informed of the results with each technique, possible complications and real expectations in terms of time for pregnancy to occur. Therapeutic alternatives should be mentioned so as to allow an informed decision by the couple:-
Surgery versus Assisted Reproductive Techniques
For many decades, surgical adhesiolysis was the only realistic option for an infertile patient with pelvic adhesions. After the birth of the first "test tube" baby, a revolution in assisted reproductive techniques (ART) took place.
These techniques include:
-(IVF-ET) In vitro fertilization , embryo transfer
- Gamete intrafallopian transfer (GIFT) and Zygote intrafallopian transfer (ZIFT).
-Intracytoplasmic sperm injection (ICSI).
-PESA, MESA, TESA, TESE, etc.
Due to the wider availability of assisted reproductive technologies, the number of women with mechanical infertility, treated by tubal reconstructive surgery, has decreased, with most couples being referred to IVF–embryo transfer.
The increasing success of IVF has changed the way we evaluate and treat the infertile couple.
In the early 1980’s when pregnancy rates per cycle of IVF were less than 10%, surgery played a major role in the treatment of the infertile female.
However, the success of IVF has increased dramatically over the years, so by 1990, pregnancies occurred in one of every six cycles and by 1999, in nearly one of every three cycles. As the success of IVF has increased, the role of surgery has decreased.
Reported pregnancy rates after surgical treatment of pelvic adhesions vary from 25% to 75%. The 37% (average) rate of normal pregnancy reported after surgical treatment of moderate disease is comparable to the clinical pregnancy rate of 30% to 55% per IVF-ET.
My own comparative results
Laparoscopic adhesiolysis PR% (two years follow-up):
- Mild : 65%
- Moderate: 35%
- Severe : 22%
ART Pregnancy rate (clinical pregnancy rate per fresh Embryo Transfer):
- Patients aged 35 years and less 65.2%
- Overall PR 50.6%
However, if you take 6 cycles cumulative pregnancy rate of IVF, versus 6 postoperative adhesiolysis pregnancy rate, IVF certainly comes out far better. While it is tempting to relegate infertility surgery and the infertility surgeon to history of gynaecology, such a move would clearly be wrong. Surgery is still necessary and indicated in several clinical situations.
An example of relatively simple, effective surgery is the laparoscopic excision of delicate, avascular adhesions encasing the ovary or the distal end of an otherwise normal fallopian tube. Recent series of salpingolysis or salpingoovariolysis report success rates up to 70%. Even when there are severe peritubal or fimbrial adhesions, cumulative pregnancy rates after laparoscopic fimbrioplasty are higher (51.4%) than those typically achieved through a single cycle of IVF in most programs and at less cost.
The decision whether to perform tubal surgery or IVF depends on several factors:-
Before choosing between surgery and ART, one must consider the following:
Tubal mucous layer (intra-tubal adhesions and folds): The degree of tubal mucosa damage is the most important prognostic factor in tubal surgery.
Tubal wall: thickness
- The patient's age.
- Previous reproductive surgery??.
- Condition of the tubes
- Severity of adhesions (type and size) extensive and dense adhesions have a poor prognosis of surgery
- Coexistent infertility factors, for example: poor semen, suspected cervical or immunological causes.
- Experience of the surgeon.
- The success rate of IVF.
- The financial constraints.
- And last, but not least, the couple’s wishes.
The role of laparoscopic Surgery in an in vitro fertilization program:
Even in cases when IVF is the right choice, laparoscopic surgery has an important role to play.
It is the duty of the surgeon to make sure that the ovaries are accessible for oocyte pickup by the transvaginal route, by performing adhesiolysis in cases where the ovaries are inaccessible vaginally. The techniques of tubal translaparoscopic transfer of gametes or embryos (gamete intrafallopian transfer (GIFT), tubal embryo transfer (TET), zygote intrafallopian transfer (ZIFT), etc.) are nearly obsolete. Methods of transvaginal ambulatory embryo transfer, which give comparable results, are definitely less invasive.
The surgeon must also remove any tube with hydrosalpinx, as it lowers the success rates in IVF. Salpingectomy performed for hydrosalpinx, prior to IVF, improves pregnancy rate, implantation, and live birth rates.
Adjuvants for adhesion reduction.
Methods that decrease adhesions:
- Inhibiting the coagulation cascade and promoting fibrinolysis.
- decrease inflammatory response
- Using barriers for separation of surfaces at high risk for adhesion formation.
1. Fibrinolytic agents (fibrinolysis , plasminogen activators stimulation)
Fibrinolysin, Streptokinase, Urokinase, Hyaluronidase, Chymotrypsin, Trypsin, Pepsin
Plasminogen activators
2. Anticoagulants (prevention of clot and fibrin formation)
Heparin, Citrates, Oxalates
3. Anti-inflammatory Agents (reduce vascular permeability, decrease histamine release and, lysozomes stabilisation)
Corticosteroids, Nonsteroidal anti-inflammatory agents, Anti-histamines, Progesterone Calcium channel blockers, Colchicine
4. Antibiotics (prevent infection)
Tetracycline, Cephalosporin
5. Mechanical Separation (surface separation and hydro flotation)
- Intra-abdominal Instillates:
Dextran, Mineral oil, Silicone, Vaseline, Crystalloid solutions, Carboxymethylcellulose
Hyaluronic acid, Chelated hyaluronic acid, Poloxamer, Icodextrin 4%
- Barriers:
Endogenous tissues:
Omental grafts, peritoneal grafts, Bladder strips, fetal membranes
Exogenous materials:
Fibrin glue ,Polytetrafluoroethylene ,Oxidized cellulose ,Oxidized regenerated cellulose Gelatin ,Rubber sheets ,Metal foils ,Plastic hoods
The most popular strategy used for adhesion reduction is the use of crystalloid solutions to irrigate (Hydroflotation) during surgery (open or laparoscopic) and instillation into the peritoneal cavity at the end of surgery in sufficient volume (300-500 ml) to allow for 'flotation' of the abdominal and pelvic organs. Physiological crystalloid solutions – saline, Ringer's lactated solution and Hartman's solution are frequently used. Their attraction may lie in their simplicity of use, availability and are relative inexpensive.
However, these crystalloids are rapidly absorbed. These solutions are absorbed from the peritoneal cavity at the rate of 30 - 60 ml per hour, so that 10 -12 hours after surgery, little, if any, crystalloid structure would be left in the pelvis.
Peritoneal healing may take as long as 5 - 7 days, thereby meaning that there is an extended period of time during which fibrin outpouring from the damaged surfaces can interconnect with adjacent structures in the peritoneal cavity, leading to adhesion formation. Therefore, post surgical instillates with prolonged peritoneal residence time should theoretically be more successful at preventing adhesions.
A more vicious gel preparation has been developed: Intergel solution ( ionically cross-linked 0.5% ferric hyaluronic acid), (Gynecare, USA), which has an increased residence time in the peritoneal cavity.
Another Preparation: Icodextrin 4% (Adept) (Shire pharmaceuticals, UK) is colourless, non-viscous and iso-osmolar with an intraperitoneal residence time of at least 4 days.
The significance of good surgical technique
Adhesions are most likely to form following tissue ischemia caused by surgical knots and the opposition of damaged peritoneal surfaces.
Recent studies have shown that it is not necessary to suture the peritoneum to help it heal after surgery. Indeed, it is better to leave the peritoneum unsutured. It will heal satisfactorily with fewer adhesions (suturing causes inflammation and foreign body reaction to suture material and may lead to tissue ischemia)
It is essential to use gentle techniques when operating on the ovary and copious irrigation to prevent tissue drying.
It is also important to be careful about haemostasis since the presence of blood in the peritoneal cavity increases the likelihood of postoperative adhesions.
It is also important to be careful about haemostasis since the presence of blood in the peritoneal cavity increases the likelihood of postoperative adhesions.
Excessive use of electro surgery can cause substantial tissue necrosis.
The bad effects of bad surgical technique cannot be avoided by any liquid barrier.
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
