Diagnosis and Prevention of Cervical Cancer - Human Papillomavirus infection
Human Papillomavirus (HPV) is the main cause of most of the histological changes that affect the female reproductive tract that includes the vagina, cervix, external genitalia, and the anus.
HPV is considered the most common cause of the cervical CA that’s why we are going to talk about it.
Human Papillomavirus (HPV)
This is a DNA virus that infects the skin and the mucosal membranes. And there are more than 100 types of HPV and some of these viruses cause skin polyps and that why its named a papillomavirus , and its transmitted by skin to skin contact and there is around 30 types that is transmitted sexually. Genital HPV is very common and it infects around 75% of women in west countries through out there entire life.
General characteristics of Human Papillomavirus




- It's part of papillomaviridae family that can be fully integrated with the DNA of the host cell. Humans are the only known source of this virus.
- There is more than 100 types of HPV that have different DNA sequences and there specific group called genital HPV that are dangerous especially HPV 16, 18, 31, 45, 58 in addition to HPV 33, 35,39, 51, 52, 56, 59, 68, 73, 82 that are known as an important factor for development of cervical cancer.
Signs and symptoms of infection with Human Papillomavirus:
- Skin polyps:
- - Common warts
- Planter warts
- Flat warts, and this is found mainly on the arms, face, and forehead.
- Nail warts
- - Common warts
- Anogenital warts (condylomata acuminata):
90% of cases are caused by HPV 6 and 11, and usually the infection with this virus is resolved spontaneously without appearance of warts or any other signs or symptoms and its worth mentioning that the virus types that cause the genital warts don’t cause cervical cancer. - Respiratory papillomatosis:
HPV type 6 and 11 can cause a rare condition called recurrent respiratory papillomatosis in which the warts are formed in the larynx and other parts of the trachea and those warts can recur many times and it may need multiple surgeries and it can hinder the respiration and in extremely rare cases it might develop to cancer. - Cancers that are related to HPV:
There are 6 types of HPV that are classified as dangerous viruses such as HPV 16, 18, 31, 45, because they have high ability to cause cervical, anal, vaginal cancer in addition to head, neck, and penile cancer. And they have a genetic relation such as E6 and E7 that are known as carcinogens that encourage the growth of the tumor and the malignant transformation.
Methods of spread of Human Papillomavirus and prevention:
Most of people can be infected with one of those cutaneous viruses during childhood period. The HPV has protein shell (strong, enable them to stay in the environment for long period of time), therefore avoidance of touching of metallic surfaces such as toilet floors may decrease the risk of cutaneous infections. The genital infection can spread quickly through the skin of the genitalia and the mucosal membranes and it can be asymptomatic. There are multiple strategies can be followed to decrease the risk of the diseases that can be developed from the genital HPV.
- HPV Tests:
This test is done by detecting the genetic material (DNA) of the HPV. And like the Pap smear it's done on the cervical cells and it can be done at the same time as the Pap smear test. And it's done for the cases bellow:- - Women who had atypical squamous cells that considered as abnormal cervical cells in the Pap smear to check for high-risk types of HPV. And if the test shows the presence of high risk types of HPV, then further approach like colposcopy or cervical biopsy should be considered.
- In the women older than 30 years as part of abnormal cervical cells screening.
Nucleic acid hybridization test is the most sensitive method for the detection of 18 types of HPV DNA in cervical samples. And it differentiate between tow HPV groups: the low risk group that includes types 6/11/42/43/44, and the high/intermediate-risk group that includes types 16/18/31/33/35/39/45/51/56/58/59/68, but it can't detect the specific type of HPV that present.
- - Women who had atypical squamous cells that considered as abnormal cervical cells in the Pap smear to check for high-risk types of HPV. And if the test shows the presence of high risk types of HPV, then further approach like colposcopy or cervical biopsy should be considered.
- HPV vaccine:
- - Two types of HPV vaccines are available, the Cervarix and the Gardasil, both protect against HPV-16 and HPV-18 that that cause 80% of anal cancers, 70% of cervical cancers, 60% of vaginal cancers and 40% of vulvar cancer. Gardasil also protects against HPV-6 and HPV-11 that cause 90% of genital warts.
- Both vaccines are given in 3 shots over 6 months.
- It's recommended for 11 and 12 years old girls and it can be given at age of 9 years, it can be given also for girls and women at age of 13 to 26 years who have not been vaccinated or completed the vaccine series yet. And it's not recommended for women at age of more than 26 years and the best way to screen for cervical CA at this age is by doing regular Pap tests.
- It should be given for females before they become sexually active and before they are exposed to HPV, it can be given for women who are sexually active but they may get less benefit because they may have already been exposed to some HPV types targeted by the vaccine.
- It's not recommended to be given during pregnancy, although studies found that it doesn’t harm the baby, but more researches is needed. Getting the vaccine during pregnancy is not an indication to end the pregnancy.
- The vaccine can't protect against all types of cervical cancer ( about 30% of cervical cancers will not be prevented by the vaccine) , therefore it's important to continue to be screened for cervical cancer ( Pap smear regularly) even after getting all 3 shots of the vaccine.
- - Two types of HPV vaccines are available, the Cervarix and the Gardasil, both protect against HPV-16 and HPV-18 that that cause 80% of anal cancers, 70% of cervical cancers, 60% of vaginal cancers and 40% of vulvar cancer. Gardasil also protects against HPV-6 and HPV-11 that cause 90% of genital warts.
- Other ways to prevent HPV:
- - Use condoms with every time of having sex from start to finish, but HPV can infect areas that are not covered with condoms, so it not fully protect against HPV.
- To be in faithful relationship with one partner.
- Choosing a partner who had few or no prior sex partners.
- The only sure way of protection is to avoid all sexual activities.
- - Use condoms with every time of having sex from start to finish, but HPV can infect areas that are not covered with condoms, so it not fully protect against HPV.
- Avoid smoking as it increases the risk of cervical cancer.
Pap smear
The papanicolaou test (also called Pap smear) is a screening test that is used to detect the precancerous changes (cervical intraepithelial neuplasia CIN or cervical dysplasia) and the cancerous changes in the endocervical canal that are usually caused by sexually transmitted HPV, and it can also detect infections and abnormalities in the endocervix and the endometrium.
- Indications of Pap smear:
- - Screening starts in general at about the age of 20 to 25 and this vary from country to another and continues until the age of 50 or 60 and it's recommended every three to five years if the previous results were normal and more frequent Pap smear is needed after abnormal results.
- It should not be done before the age of 21 and women should not do the screening until few years have passed after their first intercourse because if they had HPV after becoming sexually active, their immune system will take about 1 to 4 years to control this infection, so screening during this period may show mild abnormalities that are related to this immune reaction and not to the cervical cancer and this will cause stress to the woman and may lead to further investigation that are not necessary. And as the developing of cervical cancer usually take long time, so delaying the screening test for the reason mentioned above will carry a very little risk of missing a precancerous lesion.
- Pap smear is indicated even for those women who had the HPV vaccine because it doesn’t cover all the HPV types that cause cervical cancer.
- There is no need to screen:- - Women who haven’t had sexual contact before.
- Women aged 60 or over if there last 3 Pap smears were normal.
- Women after complete hysterectomy for benign disease.
- - Women who haven’t had sexual contact before.
- - Screening starts in general at about the age of 20 to 25 and this vary from country to another and continues until the age of 50 or 60 and it's recommended every three to five years if the previous results were normal and more frequent Pap smear is needed after abnormal results.
- Types of Pap smear:
- - Conventional Pap: after collecting the sample, it smeared directly on to microscopic slide.
- Liquid based Pap: the collected sample is put in a liquid to be preserved until it transferred to the lab then it smeared on to the slide.
- - Conventional Pap: after collecting the sample, it smeared directly on to microscopic slide.
- Procedure for taking Pap smear:
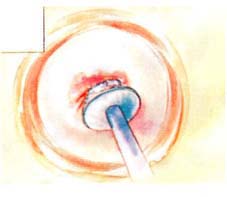
- - It starts by inserting a speculum in to the vagina then open it to allow an access to the cervix, the sample of cells is collected from the outer opening of the cervix by a spatula. Then an endocervical brush is rotated inside the cervical opening and the collected cells are placed on a glass slide then it's taken to the lab.
- It's advised not to do the Pap smear during menstruation because the blood and the endometrial cells may obscure cervical cells.
- It's not painful procedure and using small amount of water-based gel lubricant does not interfere with the result.
- The sample is stained using papanicolaou technique.

Position for taking cervical smear
- - It starts by inserting a speculum in to the vagina then open it to allow an access to the cervix, the sample of cells is collected from the outer opening of the cervix by a spatula. Then an endocervical brush is rotated inside the cervical opening and the collected cells are placed on a glass slide then it's taken to the lab.
- Results:
- - Most Pap smear results are normal.
- 2-5% are mildly abnormal and this includes:- ASC-US: atypical squamous cells of undetermined significance.
LSIL (CIN 1): low grade squamous intraepithelial lesion.
- Both indicating HPV infection.
- Although most of the low grade cervical dysplasia can regress spontaneously without causing cervical cancer, but precaution should be taken.
- 0.5% of cases are high grade SIL (HSIL) (CIN2/3), High Grade Cervical Intraepithelial Lesion.
- Less than 0.5 % indicate cancer ( squamous cell carcinoma)
- 0.2%-0.8% indicates Atypical Glandular Cells of undetermined Significance (AGC-NOS). - ASC-US: atypical squamous cells of undetermined significance.
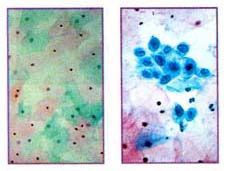
Normal PAP smear Abnormal PAP smear
- - Most Pap smear results are normal.
Cervical intraepithelial neoplasia:
CIN is a premalignant transformation of cervical squamous cells and it's not a cancer, most of CIN cases remain stable or are cured by the immune system. Small percentage of cases might progress to cervical cancer if untreated.
Most common cause of CIN is human papillomavirus (HPV) especially the types 16 and 18. And its diagnosed by the Pap smear screening test, and if it was abnormal , then colposcopy of cervix is recommended.
- Classification of Cervical intraepithelial neoplasia:
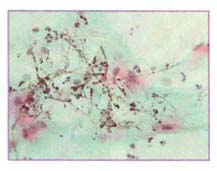
Candidiasis in a pap smear
- - CIN 1(LSIL):
- - Mild dysplasia restricted to basal 1/3 of epithelium.
- Its caused by HPV infection
- Usually cleared by the immune system in a year or more.
- CIN 2/3(HSIL):- - CIN2: moderate dysplasia in basal 2/3 of epithelium
- CIN3: severe dysplasia that involves more than 2/3 of epithelium an it may extends to involve the full thickness and this is called cervical carcinoma in situ
- - Mild dysplasia restricted to basal 1/3 of epithelium.
- - CIN 1(LSIL):
- Treatment of Cervical intraepithelial neoplasia:
- - CIN1 need no treatment if it last less than 2 years.
- CIN of higher grade requires treatment that includes destruction of abnormal cells by cervical conization, laser cautery, loop electrical excision, electrocautery or cryocautery.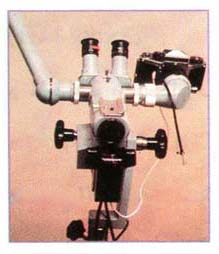
- - CIN1 need no treatment if it last less than 2 years.
- Colposcopy:
- - It’s a diagnostic procedure that is used to examine magnified view of cervix to distinguish the normal from the abnormal tissues then direct biobsies will be taken from the abnormal areas for pathological examination.
-Indications of Colposcopy:- - Pap smear shows abnormality that indicates cervical dysplasia or cancer
- Evidence of HPV
- Pap smear shows repeated atypical squamous cells of undetermined significance (ASCUS).
- If there is history of exposure to prenatal DES.- It is also done if the cervix looked abnormal during collection of the Pap smear.
- It is a simple procedure and doesn’t require anesthesia and it takes about 10 minutes.
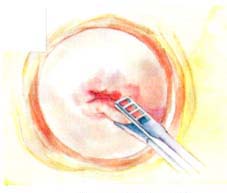
-How is colposcopy done:- - It starts first by examining the vulva and the vagina for the presence of warts or any abnormal growth. Then the speculum is inserted and the pap smear will be taken.
- Then the cervix will be inspected , and the squamocolumner junction must be seen which is the area in which most cases of cervical cancer arise , and it’s the area between the squamous and columner cells the form the endocervical canal that connects the cervix to the uterus. After menopause this area tends to migrate inside the endocervical canal and therefore colcoscopy is usually not adequate after menopause and in those cases another procedures can be done to examine this squamocolumner junction such as cold knife and cold biopsy.- - Tests done during colposcopy:
- Acetic acid wash: this chemical used to wash the cervix which is diluted 3% to 5% that wash the mucus in the cervix and it will stain the abnormal areas white (acetowhite lesions), some times normal areas can be stained white but it will have faint borders while the abnormal areas will have clear borders.
- Staining with lugol's solution: and this solution is a diluted iodine solution that can be used to distinguish the normal cells that will be stained brown when exposed to this solution from the abnormal areas that will not be stained.
- Color filters: these filters , green or blue filtered light, can be used to distinguish the tiny blood vessels ( the abnormal capillaries) inside the acetowhite area which appear as red spots or in a pattern as hexagonal floor tiles, while the normal capillaries are slender with regular spaces.
- Cervical biopsy: biopsies is taken from the abnormal areas and then the treatment will be decided according to the result of the biopsy.
- Treatment according the result of the colposcopy:
- Treatment is recommended if the biopsy show pre-cancer (dysplasia) or cancer.
- There are 2 types of treatment, ablation and resection and both types cure 90% of patients with mild dysplasia.
- Ablation which is the destruction of the abnormal area is used in the mild dysplasia and it includes Carbone dioxide laser photo ablation and cryocautery.
- Resection which is the removal of the abnormal areas is used in the more severe dysplasia and cancer and this includes loop electrosurgical excision procedure (LEEP), cold knife conization, and hysterectomy.
- CO2 laser photo ablation: this laser will vaporize the abnormal area , in less than 1% complication can occur that includes cervical stenosis or delayed bleeding.
- Cryocautery: this includes freezing the abnormal areas by using nitrous oxide and in less than 1% complication can occur that includes cervical stenosis or delayed bleeding.
- Loop electrosurgical excision procedure (LEEP): this uses a radiofrequency current to remove the abnormal areas and complication occur in 1-2% and this includes cervical stenosis and bleeding.
- Cone biopsy: it is used in the cases when the area cant be viewed during the colposcopy and also its used to obtain special sample in more advanced abnormalities and it associated with higher complication rate than other procedures, in around 5% of cases bleeding may occur post op and it may cause narrowing of the cervix.
- Hysterectomy: this is a surgical removal of uterus and its done in all cases of invasive cervical cancer and also if dysplasia recurred after any other treatment procedure and sometimes its done to treat severe dysplasia.
- - Tests done during colposcopy:
- - Pap smear shows abnormality that indicates cervical dysplasia or cancer
- - It’s a diagnostic procedure that is used to examine magnified view of cervix to distinguish the normal from the abnormal tissues then direct biobsies will be taken from the abnormal areas for pathological examination.
 electro - surgical loop ( LLETZ ) -
electro - surgical loop ( LLETZ ) -
 Cervical biopsy
Cervical biopsy
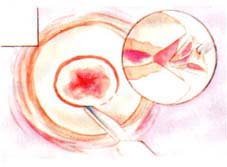 Cone biopsy
Cone biopsy
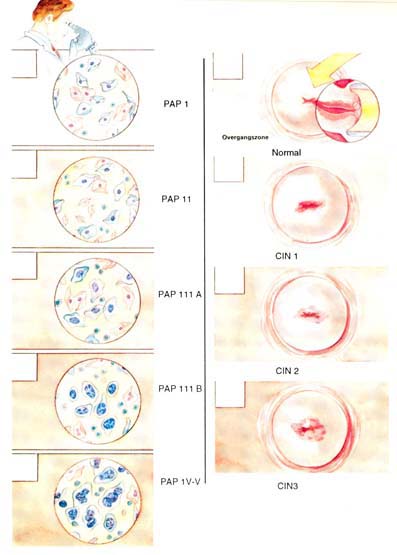 PAP and Colposcope Cervical Changes
PAP and Colposcope Cervical Changes
Dr Najeeb Layyous F.R.C.O.G
Consultant Obstetrician, Gynecologist and Infertility Specialist







 Pregnancy Due Date Calculator
Pregnancy Due Date Calculator
 Chinese Gender Predictor
Chinese Gender Predictor
 Ovulation Calculator
Ovulation Calculator
 IVF Due Date Calculator
IVF Due Date Calculator
